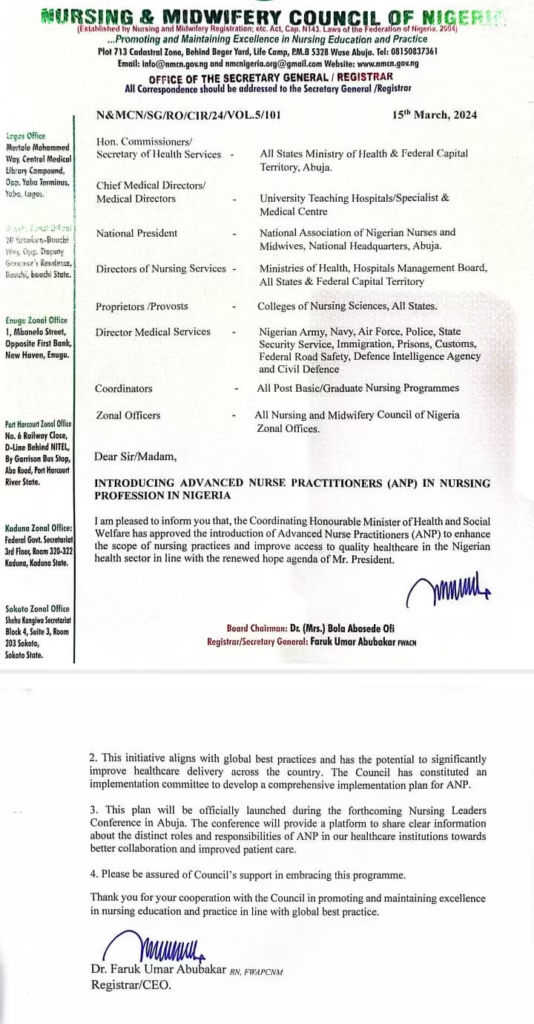
One year ago, the Nursing and Midwifery Council of Nigeria (NMCN) proudly announced the approval of the Advanced Nurse Practitioner (ANP) role—a move that was supposed to revolutionize nursing practice in the country. The approval, backed by the Coordinating Minister of Health and Social Welfare, Prof. Muhammad Ali Pate, was presented as a game-changer that would expand nurses’ scope of practice, improve healthcare access, and align Nigeria with global best practices.
According to the circular, signed by the then registrar of the Nursing and Midwifery council of Nigeria, Dr Faroq Umar Abubakar, the plan will be launched during the 2024 nursing leadership conference.

Fast forward to March 2025, the ANP role remains nothing more than a policy statement on paper. Despite all the fanfare surrounding its approval, the Nigerian nursing profession is still waiting for any tangible progress. No clear policies, no training programs, no licensing framework—just another empty promise in a healthcare system notorious for slow reforms and bureaucratic stagnation.
A Year of Inaction: Who Is to Blame?
The failure to implement the ANP role raises serious questions about the credibility of nursing and healthcare leadership in Nigeria. How can an initiative be approved without a concrete plan for execution? If this was meant to be a genuine reform, why has there been no progress in 12 months?
Here’s what’s likely behind this disgraceful delay:
1. Nursing and Midwifery Council of Nigeria (NMCN): Failing in Its Duty
The NMCN, the regulatory body responsible for nursing practice in Nigeria, has yet to produce a clear roadmap for the ANP role. Nurses still don’t know:
- What the scope of practice will be.
- How ANPs will be trained, licensed, and integrated into the system.
- What kind of educational programs will be introduced to produce qualified ANPs.
Instead of providing leadership, the NMCN has chosen silence and inaction—a familiar pattern in Nigerian regulatory bodies.
2. Government’s Empty Promises on Healthcare Reform
The government frequently makes grand declarations about improving healthcare, yet implementation is always conveniently forgotten. The ANP role was meant to expand healthcare access, especially in underserved areas. But, like many other policies, there was no real political commitment beyond the initial approval.
If the Coordinating Minister of Health and Social Welfare truly believed in this initiative, where is the budget? Where are the training centers? Where is the implementation plan?
3. Resistance from the Medical Establishment
Let’s be honest: Nigerian doctors have historically resisted expanding nurses’ roles. Many see the ANP role as a threat rather than an opportunity for a more efficient healthcare system. Instead of fostering collaboration, medical leadership in Nigeria often prioritizes professional gatekeeping over patient care.
Without political backing, nurses have been left to fight for their own advancement—a battle they seem to be losing once again.
The Consequences of This Failure
The continued delay of the ANP role is a betrayal of Nigerian nurses and patients. Here’s what it means in real terms:
- Nurses remain underutilized and unempowered, stuck in outdated roles while the rest of the world moves forward.
- Patients in rural and underserved areas continue to suffer due to the shortage of healthcare providers.
- Nigerian nurses lose international credibility, as the country fails to align with global best practices.
What Needs to Happen NOW
Enough of the excuses. If the Nigerian government and NMCN are serious about implementing the ANP role, they must:
- Immediately publish a policy framework outlining the scope of ANP practice.
- Roll out accredited ANP training programs in universities and nursing schools.
- Secure funding and political support to ensure the sustainability of the program.
- Engage stakeholders, including nursing leaders, medical associations, and policymakers, to remove unnecessary roadblocks.
Final Thoughts
Nigeria’s healthcare system is in crisis. Instead of acting with urgency, those in power have allowed bureaucracy, professional politics, and a lack of vision to stall a reform that could save lives.
If one year is not enough to implement a single nursing role, what hope is there for larger healthcare reforms? The failure to launch the ANP role is not just a delay—it’s a disgrace. It’s time for nurses to demand accountability and action.